Prostatitis

Prostatitis is a common yet frequently misunderstood urological condition that affects the prostate gland, a key component of the male reproductive system located just below the bladder. Its primary function is to produce and secrete a fluid that constitutes part of the semen. Prostatitis can cause a variety of symptoms and significantly impact quality of life, but understanding its nuances can lead to better management and treatment.
What is Prostatitis?
Prostatitis encompasses a group of conditions that involve inflammation of the prostate gland. It is categorized into several types, each with different causes and symptoms:
- Acute Bacterial Prostatitis: This is the least common but most severe form. It is caused by a bacterial infection and can lead to severe urinary symptoms and other systemic symptoms such as fever and chills. It requires immediate medical attention.
- Chronic Bacterial Prostatitis: Similar to the acute version, this form is caused by bacterial infections but the symptoms are less severe and can fluctuate in intensity over a period of months.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): This is the most common type of prostatitis, accounting for around 90% of the cases. The symptoms can include pelvic or perineal pain without evidence of urinary tract infection.
- Asymptomatic Inflammatory Prostatitis: In this type, men do not report symptoms (asymptomatic) despite having inflammation of the prostate gland. It is often discovered incidentally during examinations for other conditions.
How Prostatitis Affects Men
The impact of prostatitis on men can vary widely depending on the type and severity. Symptoms may include:
- Painful, difficult, and/or frequent urination
- Pelvic, abdominal, or lower back pain
- Painful ejaculations
- Flu-like symptoms (especially in acute bacterial prostatitis)
- Chronic fatigue and discomfort
These symptoms can lead to significant distress, affecting emotional and psychological health. Men may experience anxiety and depression, particularly with chronic forms of prostatitis, where the pain and discomfort can be persistent and debilitating.
Diagnosis and Treatment
Diagnosing prostatitis involves a combination of clinical evaluation, including a detailed medical history and physical examination, along with laboratory tests which may include urine tests, blood tests, and possibly a prostate secretion test. Imaging studies and biopsies may be used in complex cases.
Treatment depends on the type of prostatitis:
- Acute Bacterial Prostatitis is treated with antibiotics, and sometimes requires hospitalization if the symptoms are severe.
- Chronic Bacterial Prostatitis may require a longer course of antibiotics, and treatment is generally successful, although recurrence is common.
- Chronic Pelvic Pain Syndrome may be more challenging to treat, with a combination of medications, physical therapy, and sometimes more experimental treatments being employed.
- Asymptomatic Inflammatory Prostatitis generally does not require treatment unless it is affecting fertility or is involved in other complications.
Lifestyle modifications, such as increasing fluid intake, modifying the diet, and reducing stress, may also help manage symptoms.
Statistics and Epidemiology
Prostatitis is a prevalent condition among men of all ages but is most common in adults over 30. According to the U.S. National Institutes of Health (NIH), it accounts for about 25% of all office visits involving the genital and urinary systems from young and middle-aged men. It is estimated that 50% of men experience symptoms of prostatitis at some point in their lives.
Studies show that prostatitis can affect men's quality of life to a degree similar to conditions like ischemic heart disease or diabetes due to the chronic pain and discomfort it often causes.
Conclusion
Prostatitis is a multifaceted disease that can significantly affect a man's quality of life. Understanding the different types of prostatitis and their respective treatments is crucial for effective management. Ongoing research continues to evolve our understanding and treatment approaches, offering hope for better management strategies in the future.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH. "Prostatitis: Inflammation of the Prostate." https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate
- Mayo Clinic. "Prostatitis." https://www.mayoclinic.org/diseases-conditions/prostatitis/symptoms-causes/syc-20355766
- American Urological Association
Top picks
-
Kegel Pelvic Floor Muscle Trainer for Men
Regular price $99.00 USDRegular priceUnit price / per$149.00 USDSale price $99.00 USDSale -
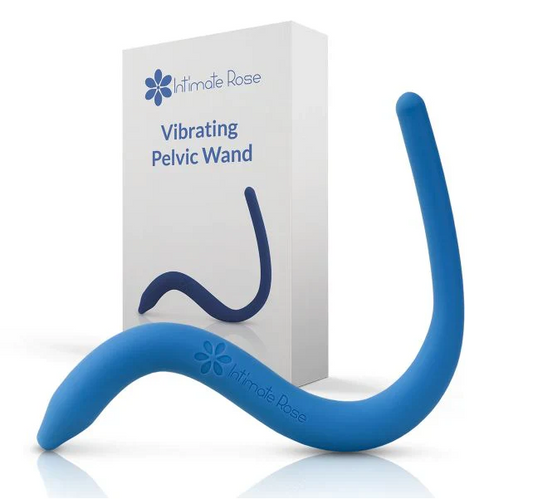
Pelvic Floor Wand & Massage Therapy Tool for Men
Regular price $49.95 USDRegular priceUnit price / per$59.95 USDSale price $49.95 USDSale -
Prostate and Pelvic Floor Support Cushion – Large Black Seat for Pain Relief
Regular price $49.95 USDRegular priceUnit price / per$75.50 USDSale price $49.95 USDSale -
Sonic Prostate Massager from Prostate Health Center | Ultimate Prostate Wellness Tool | Top-Rated Home Prostate Massage Device
Regular price $59.95 USDRegular priceUnit price / per$79.99 USDSale price $59.95 USDSale