Internal Pelvic Floor Physical Therapy

Aug 1, 2024 | 27 min read
Author: Slava Romanski
Internal pelvic floor physical treatment is a specialized treatment centering on the often-overlooked pelvic floor muscles. These vital muscles bolster pelvic organs, control bladder and bowel work, and contribute to sexual wellbeing. Shockingly, numerous individuals do not look for offer assistance until side effects like incontinence, pelvic torment, or sexual brokenness arise.
The term "inner pelvic floor physical treatment" alludes to helpful intercessions including coordinate control and treatment of the pelvic floor muscles by means of the vaginal or rectal canal. This approach is vital for diagnosing and treating conditions that outside evaluations cannot satisfactorily address. The treatment is custom fitted to each patient’s needs, tending to issues such as muscle shortcoming, snugness, or coordination problems.
This article investigates the life systems and work of the pelvic floor, the nitty gritty handle included in inside pelvic floor physical treatment, the conditions it treats, and the results patients can anticipate. We moreover examine who can advantage from this treatment and give direction on looking for fitting treatment.
Comprehending the Pelvic Floor
The pelvic floor acts as a support system for the pelvic organs, such as the bladder, intestines, and uterus in women, made up of muscles, ligaments, and connective tissue in a hammock-like structure. The pelvic floor muscles play a crucial role in upholding continence, offering support for organs, and aiding in sexual function.
Structure and Role of the Pelvic Floor
The deep pelvic diaphragm muscles and the superficial perineal muscles comprise the two main layers of the pelvic floor muscles. Deep muscles include the coccygeus muscle and the levator ani group, which includes the pubococcygeus, puborectalis, and iliococcygeus muscles. Maintaining continence and elevating the pelvic floor are the responsibilities of these muscles.
Muscles such as the bulbospongiosus, ischiocavernosus, and the superficial transverse perineal muscles are part of the superficial layer. These muscles play a role in regulating urination, ejaculation in males, and orgasm in both genders. They also help support the function of the pelvic floor during actions such as coughing, sneezing, and lifting heavy items.
Specialist Prostate Health Outlet
Differences Between Male and Female Pelvic Floor
Men and women have quite different pelvic floor structures because of their different reproductive systems. For women, the pelvic floor is very important because it supports the bladder, uterus, and rectum and allows the urethra, vagina, and anus to function properly. This area is heavily affected during pregnancy and childbirth, which can result in issues like incontinence or leakage.
On the other hand, the male pelvis supports the bladder and rectum, and is located in the prostate gland. Pelvic floor problems in men can result from things like prostate surgery, chronic constipation, or participation in high-impact sports. Understanding these anatomical differences is important in order to tailor pelvic floor therapies to address gender-specific concerns.
Pelvic Floor in Daily Life
Your pelvic floor is working hard in many daily activities and you don’t even know it. They contract when you do activities that increase abdominal pressure such as lifting, coughing or sneezing to maintain continence. They also play a big role in sexual function, contracting rhythmically during sex to help with arousal and orgasm.

And they work with your core muscles (diaphragm and abdominal muscles) to support your posture and your spine. This team work is the foundation of most physical activities and overall physical health.
Internal Pelvic Floor Physical Therapy: What to Expect
Internal pelvic floor physical therapy begins with a comprehensive evaluation, including a thorough medical history and a detailed examination. The assessment helps identify the underlying causes of pelvic floor dysfunction, whether they are related to muscle weakness, tightness, or coordination issues.
Specializing in Prostate Health Products
Initial Assessment and Diagnosis
The first test is both external and internal. The external exam looks at posture, breathing patterns and the activity of the abdominal and pelvic muscles. This helps identify any external factors that may be contributing to pelvic floor dysfunction such as poor posture or breathing patterns.
An internal exam with the patient’s consent involves inserting a gloved finger into the vagina. This allows for direct assessment of tone, strength, muscle tone of the pelvic floor and any areas of pain or tenderness. The therapist may ask the patient to do certain things such as contracting or relaxing the pelvic floor muscles to test function.
Procedures and Strategies Utilized in Inner Pelvic Floor Physical Therapy
Internal pelvic floor physical treatment incorporates a assortment of strategies custom-made to the patient's particular needs. These can include:
Patient Experiences and Expectations
Patient experiences with internal pelvic floor physical therapy vary widely, but the therapy can be life-changing for many. Patients often start therapy with specific goals, such as reducing incontinence, alleviating pain, or improving sexual function. The process can be gradual, with improvements seen over weeks or months.
Therapists work closely with patients to ensure they feel comfortable and supported throughout the process. Open communication is encouraged, and patients are urged to discuss any discomfort or concerns they may have. The therapeutic relationship is based on trust and mutual respect, with the therapist providing education and guidance and the patient taking an active role in their treatment.
Safety and Comfort Considerations
Internal pelvic floor physical therapy is generally safe but make sure you are comfortable and safe. The therapist should explain everything to you and get your consent before doing any internal exam or treatment. You can ask questions, express concerns and stop treatment at any time if you feel uncomfortable.
Benefits and Outcomes
The benefits of internal pelvic floor physical therapy are multifaceted, encompassing physical, emotional, and psychological improvements. Many patients experience significant relief from symptoms such as urinary incontinence, pelvic pain, and sexual dysfunction. Improved pelvic floor function can also enhance overall physical function, including core stability and posture, which can positively impact daily activities and athletic performance.

Symptom Relief and Improved Quality of Life
Symptom relief is often one of the most immediate and noticeable benefits of internal pelvic floor physical therapy. Patients suffering from incontinence may see a reduction in episodes, while those with pelvic pain may experience significant pain relief. Improvements in sexual function, such as reduced pain during intercourse or increased sensation, are also common outcomes.
Beyond the physical benefits, internal pelvic floor physical therapy can significantly enhance a patient's quality of life. The ability to manage or eliminate distressing symptoms can lead to increased confidence, reduced anxiety, and a greater sense of well-being. Patients often report feeling more empowered and in control of their bodies.
Long-term Benefits and Maintenance
Long-term maintenance of pelvic floor health is an essential aspect of internal pelvic floor physical therapy. Patients are typically provided with a home exercise program tailored to their specific needs, helping them maintain the benefits of therapy. Regular follow-up visits with the therapist can help monitor progress, address any new or recurring symptoms, and adjust the treatment plan as needed.
Maintaining a routine of pelvic floor exercises and incorporating healthy lifestyle habits, such as proper hydration, regular physical activity, and stress management, are crucial for long-term success. Patients are encouraged to continue practicing the techniques they learned during therapy to prevent the recurrence of symptoms.
Case Studies and Success Stories
Numerous case studies and success stories highlight the transformative effects of internal pelvic floor physical therapy. For example, one study may describe a woman who experienced severe postpartum pelvic pain and incontinence, which significantly improved after several months of therapy. Another case might involve a male patient recovering from prostate surgery who found relief from pelvic pain and urinary incontinence through targeted pelvic floor exercises and biofeedback.
These stories underscore the importance of seeking specialized treatment for pelvic floor issues and the potential benefits of internal pelvic floor physical therapy. They also highlight the diversity of conditions that can be effectively treated through this therapy, from chronic pain to postpartum recovery.
Who Can Benefit and When to Seek Therapy
Internal pelvic floor physical therapy can benefit a wide range of individuals, from those experiencing mild symptoms to those with more severe pelvic floor disorders. It is particularly beneficial for individuals dealing with urinary or fecal incontinence, pelvic pain, sexual dysfunction, and pelvic organ prolapse. It can also be an essential part of recovery after childbirth or pelvic surgery.
Optimize Prostate Health with our Exclusive Selection of Vitamins and Supplements.
Conditions and Symptoms Indicating the Need for Therapy
Some of the most common conditions and symptoms indicating the need for internal pelvic floor physical therapy include:
How to Choose a Qualified Therapist
Choosing a qualified therapist is crucial for successful treatment. Look for a therapist with specialized training and experience in pelvic floor physical therapy. They should be licensed and have a good track record of working with patients with similar conditions. A referral from a healthcare provider, such as a gynecologist or urologist, can also be valuable in finding a reputable therapist.
When selecting a therapist, consider their approach to treatment. They should prioritize patient comfort, provide clear explanations of the treatment process, and offer a supportive and respectful environment. It is also beneficial to find a therapist who is up-to-date with the latest research and techniques in the field.
When to Consider Internal Pelvic Floor Physical Therapy
If you're experiencing symptoms such as incontinence, pelvic pain, or sexual dysfunction, or if you've had a significant life event that could impact your pelvic floor (such as childbirth or surgery), it may be time to consider internal pelvic floor physical therapy. Early intervention can prevent symptoms from worsening and improve your quality of life. Don't hesitate to seek help if you're experiencing pelvic floor issues – internal pelvic floor physical therapy offers effective and non-invasive treatment options.
Discover the latest in Prostate Health Supplements.
Emerging Trends and Research in Pelvic Floor Physical Therapy
The field of internal pelvic floor physical therapy is continuously evolving, with ongoing research contributing to better understanding and treatment of pelvic floor disorders. Emerging trends include the use of advanced technologies, such as real-time ultrasound imaging and electromyography (EMG), to provide more detailed assessments of pelvic floor function.
Research is also exploring the role of pelvic floor dysfunction in other health conditions, such as low back pain, and the potential benefits of pelvic floor therapy in these contexts. Additionally, there is growing recognition of the importance of mental health in managing chronic pelvic pain, with an increasing focus on integrating psychological support into pelvic floor therapy.
The Role of Technology in Advancing Pelvic Floor Therapy
Advancements in technology have significantly enhanced the field of internal pelvic floor physical therapy. Tools like real-time ultrasound imaging allow therapists and patients to visualize pelvic floor muscles in action. This visual feedback can improve the accuracy of exercises and help patients better understand their muscle movements.
Electromyography (EMG) is another valuable tool, measuring the electrical activity of pelvic floor muscles. EMG can identify muscle imbalances and track progress over time, providing a detailed picture of muscle function. These technologies can be particularly beneficial for patients with complex conditions or those not responding to traditional therapies.
The Importance of Mental Health in Pelvic Floor Therapy
Addressing mental health is increasingly recognized as a critical component of treating pelvic floor disorders, particularly chronic pelvic pain. Conditions like chronic pelvic pain often have multifactorial causes, including physical, psychological, and emotional components. Stress, anxiety, and depression can exacerbate symptoms and hinder recovery.
Integrating psychological support into pelvic floor therapy can help address these factors. Cognitive-behavioral therapy (CBT), mindfulness techniques, and relaxation strategies can reduce pain perception and improve coping skills. A holistic approach that considers both physical and psychological aspects can enhance treatment outcomes and improve overall quality of life.
Conclusion
Internal pelvic floor physical therapy is a valuable and specialized treatment option for a wide range of pelvic floor disorders. This therapy offers a comprehensive, non-invasive approach to managing symptoms and improving quality of life. Whether you're dealing with incontinence, pelvic pain, or postpartum recovery, internal pelvic floor physical therapy can provide the support and treatment you need.
Choosing a qualified therapist and understanding the therapy process are crucial steps in achieving the best outcomes. With the right guidance and commitment to treatment, many individuals can find relief from distressing symptoms and enjoy improved pelvic health.
If you're considering internal pelvic floor physical therapy, reach out to a qualified therapist to discuss your symptoms and explore the treatment options available to you. The benefits of this therapy can be profound, offering relief from symptoms and enhancing your overall well-being.
----------------------------------------------------------------------------------------
If you found this information helpful and would like to learn more about our products, click below to access the detailed guide:
Kegel Pelvic Floor Muscle Trainer
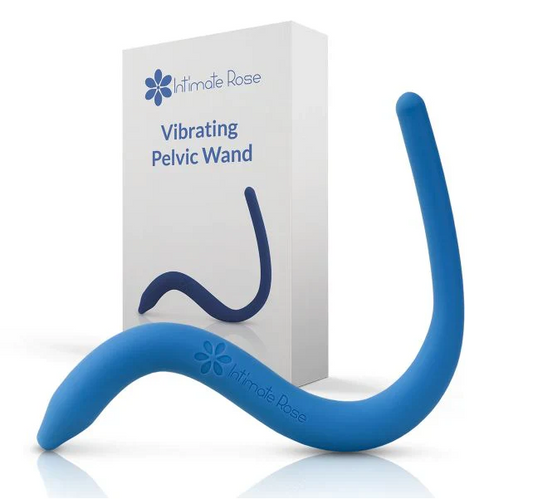
Pelvic Floor Wand & Massage Therapy
Prostate and Pelvic Floor Support Cushion
References
- Anderson, C. (2020). Pelvic Floor Physical Therapy: A Comprehensive Guide. New York, NY: Health Press.
- Bo, K., Berghmans, B., Morkved, S., & Van Kampen, M. (2007). Evidence-Based Physical Therapy for the Pelvic Floor. Elsevier Health Sciences.
- Fitzgerald, M. P., & Kotarinos, R. (2003). Myofascial Trigger Points in the Pelvic Floor. Chicago, IL: International Pelvic Pain Society.
- Hollis, H., & Dawson, A. (2016). The Pelvic Floor Bible. London, UK: Hodder & Stoughton.
- Kegel, A. H. (1948). Progressive Resistance Exercise in the Functional Restoration of the Perineal Muscles. Am J Obstet Gynecol, 56(2), 238-248.
- Simons, D. G., Travell, J. G., & Simons, L. S. (1999). Myofascial Pain and Dysfunction: The Trigger Point Manual. Lippincott Williams & Wilkins.
- Sapsford, R., & Hodges, P. W. (2001). Contraction of the Pelvic Floor Muscles During Abdominal Maneuvers. Arch Phys Med Rehabil, 82(8), 1081-1088.
Top picks
-
Kegel Pelvic Floor Muscle Trainer for Men
Regular price $99.00 USDRegular priceUnit price / per$149.00 USDSale price $99.00 USDSale -
Pelvic Floor Wand & Massage Therapy Tool for Men
Regular price $49.95 USDRegular priceUnit price / per$59.95 USDSale price $49.95 USDSale -
Prostate and Pelvic Floor Support Cushion – Large Black Seat for Pain Relief
Regular price $49.95 USDRegular priceUnit price / per$75.50 USDSale price $49.95 USDSale -
Sonic Prostate Massager from Prostate Health Center | Ultimate Prostate Wellness Tool | Top-Rated Home Prostate Massage Device
Regular price $59.95 USDRegular priceUnit price / per$79.99 USDSale price $59.95 USDSale